Share Links
UNDERSTANDING YOUR IN-LAB SLEEP STUDY RESULTS
Sleep apnea is a sleep breathing disorder that causes you to have interrupted breathing during sleep. This may cause you to sleep poorly, wake up without feeling refreshed, feel fatigued or tired during the day, experience headaches, or feel like you aren’t able to think clearly.1,2 Treatment for sleep apnea may help you feel better.
Things have advanced in sleep medicine, and many new treatment options are available beyond the classic “CPAP mask.” However, sleep apnea treatments are not one-size-fits-all. Different treatment options will be recommended by your physician depending on the severity and type of sleep apnea you have. Sleep doctors use an overnight sleep study to better understand how you are sleeping. Sleep studies used to take place in a specialized sleep lab, but more and more options are becoming available to get a study in your own home. Your doctor will discuss the results of that study—the sleep study report—with you before beginning a treatment plan. This article will focus predominantly on the results for in-lab sleep studies; home sleep tests will be covered in a future post.

What is measured in a sleep study?
- Breathing rate
- Airflow
- Oxygen levels
- Heart rate
- Brainwave activity
- Body movements
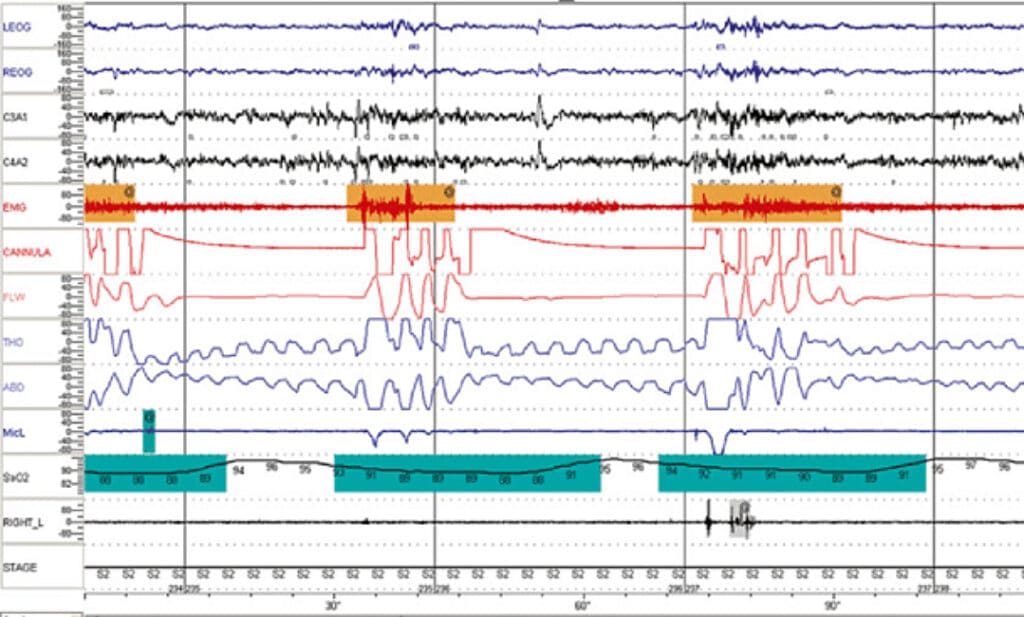
Example of sleep study monitoring data
Understanding sleep apnea severity
Beyond the short-term symptoms, sleep apnea has even been shown to increase the risk of hospitalizations and death for patients with heart failure. This may be due to the increased stress that apnea events put on your heart.7,8
- Your quality of life (as measured by various questionnaires)
- Total sleep time
- Sleep time in light sleep versus deep sleep
- Arousals and/or awakenings from sleep
- Blood oxygen levels
- Count of apneas and hypopneas
(apnea-hypopnea index)
The most common metric used to communicate sleep apnea severity with patients is the apneahypopnea
index, or AHI. This is an average of the apnea (central + obstructive + mixed) and hypopnea
events that occur during one hour of sleep. It is usually expressed as a number per hour; for example,
15 events/ hour.
Commonly used classifications are:3
Normal: AHI < 5 per hour
Mild: AHI ≥ 5, but < 15 per hour
Moderate: AHI ≥ 15, but < 30 per hour
Severe: AHI ≥ 30 per hour
Understanding the different types of apnea events
Some of the most common findings in a sleep study are apneas and hypopneas. Apneas are pauses in breathing that last at least ten seconds. Hypopneas are shallow breathing.
Apnea events are classified based on what causes the event. The main classifications are obstructive apneas, central apneas, and mixed apneas. Some clinicians may classify hypopneas as well, but there is disagreement as to the exact definitions.
OBSTRUCTIVE EVENTS
Obstructive events occur when the body tries to breathe, but a narrowing or obstruction of the breathing passages prevents air from flowing freely. This blockage, or obstruction, can be due to bodily features or a relaxation of the muscles in the chest and neck during sleep.4
CENTRAL EVENTS
Central events occurs when the brain fails to signal the breathing muscle (diaphragm) to activate. As a result, the person temporarily stops trying to breathe. Fortunately, this stoppage eventually causes the person to arouse and resume breathing, often at an increased rate.4
MIXED EVENTS
Mixed events are a combination of obstructive and central apnea. They typically begin as central apneas, then turn into obstructive once the brain activates the breathing muscles.5
What is included in my sleep report
Your sleep report will include all of the notable findings based on the information collected in the sleep study. Your physician will walk you through the details with you. We will only focus on a few key parameters below.
BREAKDOWN OF THE APNEA-HYPOPNEA INDEX
Most sleep study reports will include a breakdown of the apnea-hypopnea index (AHI) by event type. The
“Index” gives the average number of events per hour. In the example above, the patient has 11 apneas
(Central + Obstructive + Mixed) and 62 hypopneas per hour. The total AHI is 73 events/hour.
OXYGEN LEVELS IN THE BLOOD
Sleep study reports will show the number of times your blood oxygen levels dipped below certain levels (e.g. 90%). This indicates insufficient oxygen, and is often caused by the apneas and hypopneas. In the example above, the patient dropped below 90% oxygen saturation 223 times throughout the course of the study.
What happens after my sleep study?
In most cases, a sleep clinician will review your study with you and go over notable findings. The
information in your sleep study will be used to determine a treatment plan that is right for you.
Remember, different treatment options are available based on your specific type of sleep. Talk to your
doctor about which option is right for you.
Learn more

COULD THE remedē SYSTEM BE RIGHT FOR YOU?
Answer a few short questions to see if you may be a candidate.
Important safety information
The remedē® System is indicated for moderate to severe Central Sleep Apnea in adult patients.
Your doctor will need to evaluate your condition to determine if the remedē system is right for you. You will not be able to have an MRI or diathermy (special heat therapies) if you have the remedē system implanted. The remedē® System may be used if you have another stimulation device such as a heart pacemaker or defibrillator; special testing will be needed to ensure the devices are not interacting.
As with any surgically implanted device, there are risks related to the surgical procedure itself which may include, but are not limited to, pain, swelling, and infection.
Once the therapy is turned on, some patients may experience discomfort from stimulation and/or from the presence of the device. The majority of these events are resolved either on their own or by adjusting the therapy settings. The remedē® System may not work for everyone. There are additional risks associated with removing your system. If you and your doctor decide to remove the system, another surgery will be required.Be sure to talk with your doctor so that you thoroughly understand all of the risks and benefits associated with the implantation of the remedē® System. Rx only. For further information, please call +1-952-540-4470 or email info@respicardia.com.
- Costanzo MR, et al. J Am Coll Cardiol 2015; 65:72–84.
- Abraham WT, et al. Cardiac Failure Review 2018; 4(1):50–3.
- Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999 Aug 1;22(5):667-89. PMID: 10450601.
- Javaheri S., Dempsey J.A. (2013) Central sleep apnea. Compr Physiol 3:141–163.
- Dempsey J.A., et al. Pathophysiology of Sleep Apnea. Physiol Rev 90:47-112, 2010. doi:10.1152/physrev.00043.2008.

