Share Links
CENTRAL SLEEP APNEA (CSA) AND EXCESSIVE DAYTIME SLEEPINESS
Excessive daytime sleepiness (EDS) is a potential symptom of sleep apnea. This blog will focus specifically on how daytime sleepiness impacts people with central sleep apnea (CSA).
Anyone who experiences any kind of sleep apnea understands how daytime sleepiness can impact a person’s life. It goes beyond just feeling tired. Extreme daytime sleepiness can be debilitating. It can affect every part of a person’s life, from relationships to work performance. It can be a significant safety risk, as well. One study found people with excessive daytime sleepiness were 2.5 times more likely to suffer an accident at work.1
The first step in dealing with excessive daytime sleepiness is to learn more about what may be causing it.
What is Central Sleep Apnea?

Most people are familiar with obstructive sleep apnea (OSA). For people with OSA, the throat can collapse and block the airway during sleep. When that happens, the oxygen (O2) level in the blood drops, and the carbon dioxide (CO2) level rises. Sensors throughout the body alert the brain that there is a problem. The brain responds by waking the sleeper up so they will begin to breathe again.
However, OSA is just one of several kinds of apneas. Central sleep is another type of sleep apnea. For people with CSA, the signals from the brain to the breathing muscles are interrupted or irregular.2 The irregular breathing pattern leads to decreased oxygen and increased carbon dioxide in the blood. Eventually the brain senses this change and “remembers” to breathe. However, the interruptions in breathing and drops in oxygen levels can lead to poor sleep and other health risks.
One of the key symptoms of central sleep apnea is excessive daytime sleepiness. The key word is excessive. Everyone feels sleepy sometimes during the day. Not every drowsy feeling falls into the category of excessive daytime sleepiness, however.
What is Excessive Daytime Sleepiness?
EXCESSIVE DAYTIME SLEEPINESS IS WHAT DOCTORS CALL HYPERSOMNIA. IT IS DIFFERENT FROM JUST FEELING TIRED
- Can nap during the day and still feel sleepy
- Can fall asleep doing any task, even driving a car or eating
- Can still sleep a lot at night and be tired in the day
- Chronic brain fog makes it difficult to think clearly and concentrate
- Problems making decisions
- Poor short-term memory
- Lack of productivity
- Nodding off
It is hard to be subjective about something as vague as the level of sleepiness. That’s why healthcare professionals often recommend a method of self-evaluation called the Epworth Sleepiness Scale (ESS).
What is the Epworth Sleepiness Scale?
The ESS is a self-evaluation survey that can help measure levels of sleepiness.3
It lists scenarios, and the tester determines the chance they may fall asleep using this scale:
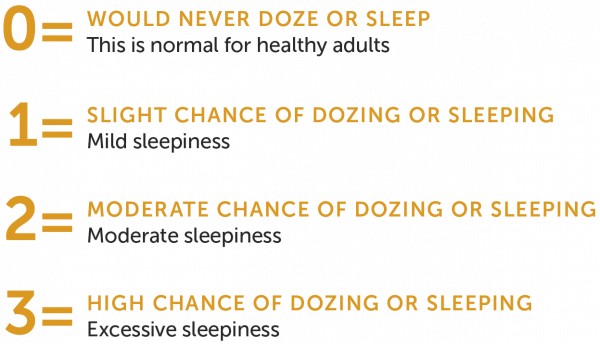
Although the test is still somewhat subjective, it gives testers a way to gauge their level of sleepiness. This test is for all kinds of sleep apnea and also for narcolepsy. Someone who scores higher than 11 on the ESS is likely experiencing excessive daytime sleepiness.3
What is the Multiple Sleep Latency Test (MSLT)?
The MSLT, which is sometimes called a daytime nap study, is a more objective survey of excessive daytime sleepiness. It measures how fast someone falls asleep in a quiet area during the day.
A board-certified sleep medicine physician conducts the MSLT. It is a full-day test that consists of five scheduled naps separated by two-hour breaks. During each nap, the subject lies quietly on a bed and tries to go to sleep. If they succeed, a staff member wakes them after 15 minutes. If they fail to fall asleep in 20 minutes, the test ends.4
During the nap, a series of sensors measure whether the person actually falls asleep and the various stages of sleep reached, such as REM. The MSLT is a clinical diagnostic test for excessive sleepiness. The ESS is a selfevaluation.
What are the Other Signs of Central Sleep Apnea?
Excessive daytime sleepiness is one of the key symptoms of CSA but not the only one. Other indicators include waking up frequently during the night or segmented sleep. Repeated pauses in breathing during sleep can disrupt sleep. Sometimes, these pauses may even cause the sleeper wakes up suddenly. Even if the sleeper doesn’t full wake up, breathing issues can make it hard to get restful sleep.
The Apnea-Hypopnea Index (AHI) measures the severity of sleep apnea based on the number of times someone stops breathing per hour during sleep:5
- Up to four times a night is normal
- Between 5-15 is mild sleep apnea
- Between 15-30 is moderate sleep apnea
- Anything greater than 30 is severe sleep apnea
Someone with severe sleep apnea could wake up 30 times or more an hour each night. That’s why someone who has CSA can feel sleepy all the time regardless of the amount of perceived sleep they get. In this case, its like someone tapping you on the shoulder all night long, telling you to “wake up and breathe”… completely exhausting!
- Morning headaches
- Shortness of breath
- Chest pain at night
- Low tolerance for exercise
How Central Sleep Apnea and Excessive Daytime Sleepiness Impact Health
The constant sleep-wake cycle takes a toll on a person mentally and physically. Sleep is a necessary part of good health. The brain uses this time to form new neural pathways that allow you to learn and remember. Studies indicate that children who do not get enough sleep have trouble at school with both learning and socialization. They may even feel angry and act out impulsively.7
People who are sleep deficient because of CSA experience brain-related side effects such as poor memory, trouble with decision-making, and problem-solving. They may struggle to control their emotions and cope with stress, as well. This all occurs because the brain didn’t have the chance to prepare for the new day.6
Central sleep apnea, when left untreated, can have serious consequences. People experiencing extreme daytime sleepiness should consider getting evaluated for central sleep apnea or obstructive sleep apnea.
Learn more

COULD THE remedē SYSTEM BE RIGHT FOR YOU?
Answer a few short questions to see if you may be a candidate.
Important safety information
The remedē® System is indicated for moderate to severe Central Sleep Apnea in adult patients.
Your doctor will need to evaluate your condition to determine if the remedē system is right for you. You will not be able to have an MRI or diathermy (special heat therapies) if you have the remedē system implanted. The remedē® System may be used if you have another stimulation device such as a heart pacemaker or defibrillator; special testing will be needed to ensure the devices are not interacting.
As with any surgically implanted device, there are risks related to the surgical procedure itself which may include, but are not limited to, pain, swelling, and infection.
Once the therapy is turned on, some patients may experience discomfort from stimulation and/or from the presence of the device. The majority of these events are resolved either on their own or by adjusting the therapy settings. The remedē® System may not work for everyone. There are additional risks associated with removing your system. If you and your doctor decide to remove the system, another surgery will be required.
Be sure to talk with your doctor so that you thoroughly understand all of the risks and benefits associated with the implantation of the remedē® System.
Rx only. For further information, please call +1-952-540-4470 or email info@respicardia.com.
- Vahid, Gharibi et al. Excessive Daytime Sleepiness and Safety Performance: Comparing Proactive and Reactive Approaches. The International Journal of Occupational and Environmental Medicine. 2020 April. https://pubmed.ncbi.nlm.nih.gov/32218557/.
- Donovan, Lucus et al. Prevalence and Characteristics of Central Compared to Obstructive Sleep Apnea: Analyses from the Sleep Heart Health Study Cohort. Sleep. 2016 Jul. https://pubmed.ncbi.nlm.nih.gov/27166235/ .
- Harvard Medical School. Narcolepsy: Epworth Sleepiness Scale. http://healthysleep.med.harvard.edu/narcolepsy/diagnosing-narcolepsy/epworth-sleepiness-scale.
- Multiple Sleep Latency Test (MSLT) – Overview and Facts. http://sleepeducation.org/disease-detection/multiple-sleep-latency-test/overview-and-facts.
- Sleep Deprivation and Deficiency. National Heart, Lung and Blood Institute. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency.
- Central Sleep Apnea. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/central-sleep-apnea/symptoms-causes/syc-20352109.
- What does “AHI” represent? American Sleep Apnea Association. 2017 Aug. https://www.sleephealth.org/ufaqs/what-is-ahi-represent/.

